Consider this my semi-annual update on the topic that non-runners stubbornly refuse to believe: The fact that running does not destroy your knees.
A new paper in Arthritis Care & Research, published by a multicenter team led by Grace Lo of Baylor College of Medicine, presents data from a long-running study called the Osteoarthritis Initiative. The findings (an earlier version of which I wrote about in 2015 when they were presented at a conference) offer some interesting new insights about the (lack of) links between running and knee osteoarthritis.
There have been plenty of previous studies that have followed groups of runners for many decades, and concluded that they were less likely to develop osteoarthritis than matched groups of non-runners (as I wrote about, for example, here). But there’s a potential flaw in these studies: Looking at people who’ve chosen to run (e.g., members of running clubs, who have featured in some of these studies) may result in an artificially healthy group of runners, because those whose knees can’t handle the pounding soon give up running and don’t join running clubs.
More From Runner's World

That’s why the new study is useful. It draws from people in the community who have no particular affiliation with running, with the goal of following them over many years, assessing them to see who develops osteoarthritis and who doesn’t, and then trying to figure out which factors play a role. The current analysis looks at 2,637 people who had medical assessments including knee X-rays, and who completed a detailed questionnaire about their exercise habits throughout their lifetime.
Of the total population, just under 30 percent reported running on a regular basis at some point in their lives. The key result is that those who reported running were less likely to report frequent knee pain, have X-ray evidence of osteoarthritis in their knees, or have symptoms of osteoarthritis compared to non-runners.
Crucially, it wasn’t just current runners who were protected; even people who reported running at some point in the past had less knee pain. That’s the opposite of what you would expect if the people who quit running did so because it was messing up their knees.
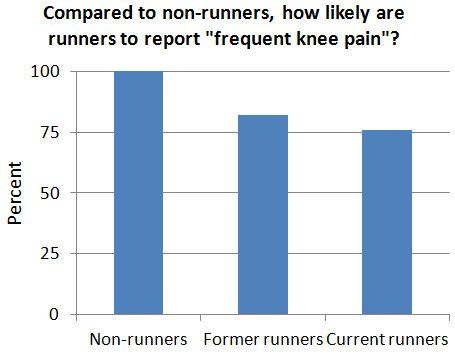
Here’s what the data looked like for frequent knee pain, which was defined as having had pain, aching, or stiffness in or around a knee for more than half the days in one month during the past 12 months. (The numbers are relative to the control group of non-runners, so "100 percent" means "just as likely as non-runners to report knee pain," and lower numbers mean the runners are less likely to report knee pain.)
Former runners were 18 percent less likely to report knee pain, while current runners were 24 percent less likely; these data were adjusted to account for differences in age, body mass index (BMI), and other factors. Without those adjustments, current runners were actually 29 percent less likely to report pain. That’s because runners tend to be lighter than non-runners, so “equalizing” BMI underestimates the benefits of running.
The results were similar for X-ray evidence of knee degeneration, and for the presence of symptomatic osteoarthritis: Having run at some point was better than nothing; current running was best of all.
Because this is an observational study with data taken at a single point in time, the authors are very careful to avoid drawing any conclusions about whether running might, in fact, help to reduce the risk of osteoarthritis. I’ll go ahead and say that there are some good reasons to think it might, primarily because it helps keep BMI low, but also potentially due to other mechanisms such as the anti-inflammatory effects of exercise (as I wrote about here last fall).
One detail that’s perhaps worth highlighting: It’s not that running made people immune from knee pain; overall, 33.0 percent of the runners reported frequent knee pain. (The average age in the study was 64.3 years old, so the prevalence of knee pain is obviously higher than it would be in, say, a bunch of college students.)
But the non-runners were even more likely to report frequent knee pain: 41.1 percent of them, overall.
That, I think, is what helps the “running ruins your knees” myth to persist: Everyone of a certain age knows someone who used to run but had to stop because their knees gave out. That sucks, but it doesn’t mean running was the cause. Look around at your non-running friends of a similar vintage, and—this and other studies suggest—you’ll find even more people with aching knees. It’s all relative, which isn’t perfect but is better than nothing.
***
Discuss this post on the Sweat Science Facebook page or on Twitter, get the latest posts via email digest, and check out the Sweat Science book!